I happily put on the hat of roving Reporter within the world of Mental Health… again.
I happily put on the hat of roving Reporter within the world of Mental Health… again.
Breaking News! POD
can build bridges between Caregivers and Patients in Psychiatric Care.
Paraphrasing from the POD website in the UK: Many people – service users, carers, and staff of all disciplines – have a strong sense that we can do better in the services we provide for people with  mental health difficulties, and the current way of working can be improved upon, towards a more holistic and collaborative approach to mental health care…. It is a less hierarchical approach, where everyone is seen as a partner in the process from day one. …peer support has been made integral to service delivery …
mental health difficulties, and the current way of working can be improved upon, towards a more holistic and collaborative approach to mental health care…. It is a less hierarchical approach, where everyone is seen as a partner in the process from day one. …peer support has been made integral to service delivery …
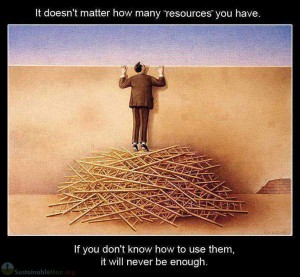
I attended a POD, Peer-Assisted Open Dialogue, Conference March 2015, in London, England. Relatively new to my awareness yet The Open Dialogue aspect has existed for over a decade in Finland. To sum up the Finnish experience: 74% of the acutely psychotic patients were either working or educating at two years. Ten times higher than the British results in a more traditional Biomedical Model of care. The Conference was a gathering together of six teams from different National Trusts, subsections of English National Healthcare System serving their geopraphic portion of the population. A Research Project to explore the POD model involving nearly twenty Psychiatrists is now underway.
A multidisciplinary team of Health Care Workers is assembled around each acute case. This could be four or more people: A Psychiatrist, A Nurse, a Psychologist, an Occupational Therapist, or any Mental Healthcare worker from  the team. A person experiencing their first case of Psychosis, although is used effectively to treat acute and non-acute cases alike, first or subsequent acute episodes, would benefit from the collaboration with the team and any friends/family members that would like to be involved (always with the Patient’s consent). Lastly, a Peer with their own personal experience of crisis within the system, is a part of this Non-heirarchical Circle. It is not always possible but the aim is not to prescribe medications until at least three meetings have occurred and with the collective agreement from the group. The Patient’s belief about medications is important and relevant in this decision. The meetings occur as frequently as deemed necessary. In acute cases this could be daily.
the team. A person experiencing their first case of Psychosis, although is used effectively to treat acute and non-acute cases alike, first or subsequent acute episodes, would benefit from the collaboration with the team and any friends/family members that would like to be involved (always with the Patient’s consent). Lastly, a Peer with their own personal experience of crisis within the system, is a part of this Non-heirarchical Circle. It is not always possible but the aim is not to prescribe medications until at least three meetings have occurred and with the collective agreement from the group. The Patient’s belief about medications is important and relevant in this decision. The meetings occur as frequently as deemed necessary. In acute cases this could be daily.
Psychiatric Upgrades of the Peer-Assisted Open Dialogue. Key points of how POD is different.
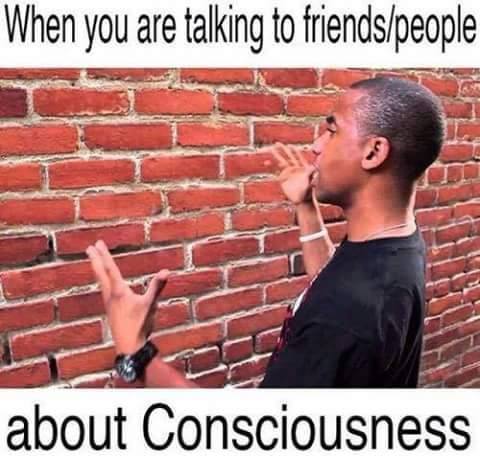
- Psychiatrists Listen to Patients – Essential to Develop a Trusting Therapeutic Alliance.
- Psychiatrists and Mental Healthcare Workers: Develop Awareness of themselves through Mindfulness Training.
- Non-Heirarchichal Healthcare Teams
A Circle: no one above, no one below. Each takes their place in the Circle.
- Peers – an Invaluable Resource.
By Peers, I mean a person who has had a similar crisis within the Psychiatric System. Also known as a former Patient. I consider as a possible translator – my own speculation.
To repeat, the key elements are:
Physician Wellness and Evolution via Mindfulness Training.
Multidisciplinary, non-heirarchal team approach.
Listening to the patient. Yes! Listen.
Too Simple to be True?
It is Simple. And it is True.
Include a Peer. Someone with experience as a Patient in Crisis.
Russell Razzaque on Breakdowns and Spirituality. 30 minute talk from the London-based Psychiatrist,  Russell Razzaque. He leads the Research Team in England.
Russell Razzaque. He leads the Research Team in England.
Open Dialogue is a System Transformation.
It is a Whole System Change.
It is about Everyone coming together in a Different Way.
Transcribed, partly Paraphrased:
Rather than try to get the Patient back to where they originally started, …perhaps there is somewhere this experience is taking the Patient.
Be open to the variation of each individual.
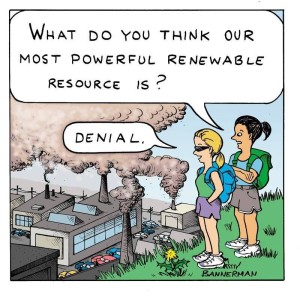
We do need a different attitude to the Suffering we have. Because it is ubiquitous to the way we run ourselves as a  Society today.
Society today.
…Epic scale of inequality we are seeing everywhere.
…Recalibrate our Relationship with Suffering.
Not something to push away or deny, try to remove and get rid of. Look at it as something that contains some Real Healing for us, as well.
Pain equals “Attention Here”.
…Wherever possible, try to find the message in pain … to learn about our True Nature.
True Nature is different for Everybody.
Enabling Everyone to have their Journey: find their Reality through their Pain. We can All Learn from each other.
My Pain takes Me to My Understanding.
Your Pain takes You to Your Understanding.
We can Respect Each Other’s Understanding.
We, as a Society, can start Learning from each other.
…Respect Everybody’s Individual Wisdom.
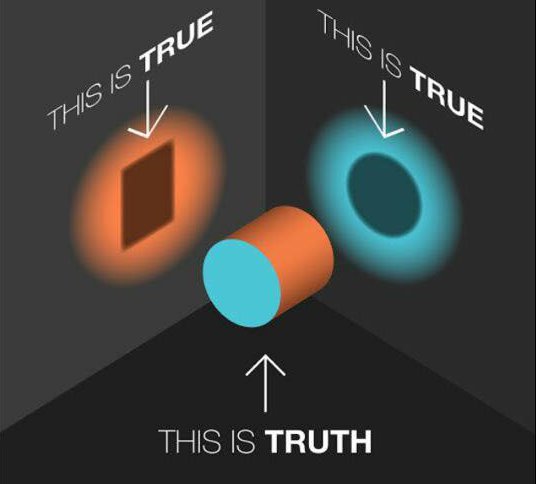
There is not One Truth that we are going to follow.
Allow everybody to have their Truth.
Practically: What to do about this?
He describes research findings: two groups of people with OOE, Out of the Ordinary Experiences. One got into the Psychiatric System ending up on Antipsychotic Medications and remained in the system for decades. The other managed to Integrate their experiences and stayed out of the Psychiatric System. Biggest difference between the two groups was that the second was surrounded by a system of Acceptance & Validation. They were Listened to and Respected.
Should not be about whether something is Real but whether it Serves a Compassionate Purpose.
Dr. Razzaque sees a day when Psychiatrists will stop being the Reality Police.
Open Dialogue, originating in Finland, is a good Avenue to start to change the way Mental Health Services are delivered.
74% of the Patients who suffered an Acute Episode of Psychosis were back to work or study at two years. And Out of the System. Ten Times higher than the results of the British Mental Health System.
 The Experimentation occurred on the backdrop of some of the worst Mental Health Services in the World, Finland. Set an environment of being willing to try something completely different.
The Experimentation occurred on the backdrop of some of the worst Mental Health Services in the World, Finland. Set an environment of being willing to try something completely different.
Everybody sits together to find meaning in what is going on. Anyone who wants to be involved is welcomed to the Process.
Open Dialogue has started to setup in various places around the World.
Four Locations starting Pilot Projects within the U.K. 50-60 Clinicians. 10-15 Psychiatrists.
Most Important thing we are teaching people is to become an Expert in Not Being an Expert. To Unlearn What We Have Learned.
…We can grow as much as anybody else through this  process.
process.
…There is no “Them” and “Us”. … All of us have Our Wounds.
We all benefit from sharing the process rather than pretending to be the Fixer: the Healer and the Wounded. It is more a relationship of Equals.
Conference March 11, 2015 in Central London 600 people registered. A lot of interest in this.
If we can Change the way we Deliver Our Mental Healthcare, it can have a Fundamental Ripple Effect on the rest of Society as a whole.
We can start to all Listen to Each Other rather than consider this is Normal, this is Not Normal.
 If someone says that a Mental Illness is just like a Physical Illness, just ask: What is the Physical Test to know that someone is Mentally Ill?
If someone says that a Mental Illness is just like a Physical Illness, just ask: What is the Physical Test to know that someone is Mentally Ill?
There isn’t one. There never has been one.
…There is no way of discerning that somebody has this physical change going on.
There is a huge debate as to whether there are actually things that are happening.
Different Schools of Thought on this. There is no clear cut answer.
Recently heard a talk from a Neuroscience Expert. There are Theories of various Chemical Imbalances. They are just Theories – Reverse-Engineered by the fact that certain drugs had effects on the Symptoms. Lots of debate on this.
Some people find some comfort to think of the Biological Illness Construct. It helps them. Then it can work.
But other people vehemently reject it. They find that it doesn’t help them.
Working with People in a way that Allows them to Lead, working on a way to Understand their Experiences – very Important.
We have to admit with some Humility that we do not have the same level of Technical Certainty that other Branches of Medicine have.
We can be in that Uncertain place and allow others to offer their input.
…This is a Grey Area. I think it is Important to Treat it as Such.
WHO, World Health Organization 10 years ago
– outcomes of Psychosis compared between Undeveloped Countries and Developed Western Countries. Relapse Rate lower in the Undeveloped Countries.
Taught in Medical School. Kind of brushed under the Carpet. Kind of Embarrassing.
When you go to those undeveloped Countries, they are doing these kinds of things (similar to Open Dialogue). …
If it works, it works. I am for anything that works for whatever person.
It will be that Person and their Belief System that helps them Define that.
 Recounted working with Patients with Violent Tendencies. Varied results: sometimes settled in 2-4 weeks, other times 2-6 months. Dr. Razzaque would ask Patients, what do you think got you better? About half of them at least said: it’s the Spirits, they are gone now. “Who am I to say that is wrong? What do I really know?” Dr. Razzaque asked himself.
Recounted working with Patients with Violent Tendencies. Varied results: sometimes settled in 2-4 weeks, other times 2-6 months. Dr. Razzaque would ask Patients, what do you think got you better? About half of them at least said: it’s the Spirits, they are gone now. “Who am I to say that is wrong? What do I really know?” Dr. Razzaque asked himself.
To Know that We Don’t Know is the most Important Thing … in terms of the Clinician.
Described Ram Dass asking his Teacher about LSD. The Teacher sampled it and felt nothing different. Even a handful of LSD doses had no impact. Was felt that he always existed in the place that LSD can take a person – a shortcut. For most people the LSD trip is not longlasting. Other methods get one there in a more permanent fashion. Taking a drug like LSD feels very violent when you exist far away from that (enlightened or expanded consciousness, my addition) place.
take a person – a shortcut. For most people the LSD trip is not longlasting. Other methods get one there in a more permanent fashion. Taking a drug like LSD feels very violent when you exist far away from that (enlightened or expanded consciousness, my addition) place.
Open Dialogue is a System Transformation. It is a Whole System Change. It is about Everyone coming together in a Different Way.
…Mindfulness also very valuable for Clinicians to own their own stuff and not let it get in the way. Not a lot of Emotional Education in Healthcare. I advocate Mindfulness (if it works for you). Voluntary.
…Recognizing your Thoughts are not who you really Are. For me, the most Important Part.
Dr. Razzaque ran a 15 minute Daily Mindfulness Practice on a Psychiatric Inpatient Ward. Open to anyone who wanted to turn up, staff or patient. The Staff did not  come, but some of the Patients did. Must be voluntary. No one can feel pressured to Engage in the Spiritual Journey.
come, but some of the Patients did. Must be voluntary. No one can feel pressured to Engage in the Spiritual Journey.
He recommends Pema Chodron’s book “Wisdom of No Escape” as it helped him.
Also notes another of her books “The Places That Scare You”.
Talking about the Messiness etc make us Who We Are. We can’t be anything unless we are all these messy things too. The Challenge is not to remove these parts of us. The challenge is to find a way to be present with them and to allow them to be as they are. We stop being dominated by the need to remove them.
*********** End Dr. Razzaque video paraphrasing.
 Author, Jeremy Wallace MD, British Trained Psychiatrist, notes, “…only by taking an approach which isn’t focused on getting to the right diagnosis, … to map the many pathways into and out of psychosis.”
Author, Jeremy Wallace MD, British Trained Psychiatrist, notes, “…only by taking an approach which isn’t focused on getting to the right diagnosis, … to map the many pathways into and out of psychosis.”
Author states: Within Psychiatry the biggest obstacle to change is the pervasive biological dogma, that is so pervasive.
I echo that sentiment as a Canadian Trained Family Doctor.
“Love is the Force”. Jaako Seikula, a Psychiatrist and one of the original Doctors in Open Dialogue in Finland. Made this statement while delivering a talk in the Medical Conference setting.
Enjoyed reading the book Spiritual Psychiatries where Natalie Tobert shared her experiences as a Medical Anthropologist.
“In India the use of a multiplicity of medical, alternative, complementary, religious and/or spiritual strategies to address human suffering is not controversial,” Tobert writes. “It is normal syncretic practice for people to try a plurality of treatments to address their well being.” The author also finds that this practice stems, at least in part, from a cultural view that sees mental illness as an almost entirely transitory state—and one that can be overcome. Natalie Tobert, Spiritual Psychiatries
Important to distinguish that Psychiatric Episodes are regarded as a transitory state in India. Alternate viable models exist. Contrasts starkly with the Biomedical Model I have experienced as both a Doctor and a Psychiatric Patient.
My Utopic Dream
Be Mindful of the Lesson. Challenge what you Believe to be True.
Fear perpetuates Fear. Stay Calm.
When you Understand your Fear, you can Act Cooperatively.
The Result: Harmony & Holistic Health.
Upgrade Normal to Optimal.
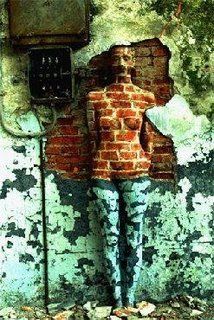
In a Nutshell: When you Treat a Bear without Understanding the Bear, it is Dangerous for both You and the Bear. The Bear represents the person in acute crisis presenting to the Mental Health System.
Brings up an important question: What is Normal?
Who gets to decide this?
To my experience, the lines are many shades of grey. Caregivers in the Inpatient system had a more black and white approach. Language used is extremely biased. New terminology use offers new opportunities for effectual communication. I am a big fan of the use of the terms shared reality and unshared reality.
Concept of Normal: not a fan. I love to consider optimal. Optimal is different for each one of us. Optimal cannot be dictated from someone else. The missing link in the Psychiatric System that I experienced as a Patient is the ability to connect to a Human Being in crisis. Despite the intentions, care feels more like imprisonment. One viable mindset holding another viable mindset captive. It does not have to continue. Excitement always rises when I consider that there are caregivers right now in different parts of the world creating Therapeutic Alliances with People in Crisis. We can argue over whether that crisis is Spiritual Emergency, Psychosis or other. Integrative Psychiatry, Transpersonal Psychology, Spiritual Emergency. I will not go into any of these terms but love that they exist as a signpost to show there may be more than one way to look at the issues. The terminology  debate continues. Perhaps there are many different processes under the same name when actually more terms are required. I do not know. I do not know is an empowering statement within any Field of Medicine. When we admit we do not know, we are open to learn. We are more likely to look with fresh eyes, heart and mind. When we wonder what is happening with our patients, we can connect to the best options for care. Medicine lumps patients into large groupings. Pragmatic, yes. Optimal. Likely not.
debate continues. Perhaps there are many different processes under the same name when actually more terms are required. I do not know. I do not know is an empowering statement within any Field of Medicine. When we admit we do not know, we are open to learn. We are more likely to look with fresh eyes, heart and mind. When we wonder what is happening with our patients, we can connect to the best options for care. Medicine lumps patients into large groupings. Pragmatic, yes. Optimal. Likely not.
Lovely that the National Health Service in England is embarking on a large study of the promising POD, Peer-Assisted Open Dialogue, style of delivering Acute Care Psychiatry. I consider what this could mean for the Acute Care System in Canada, my home at the moment.
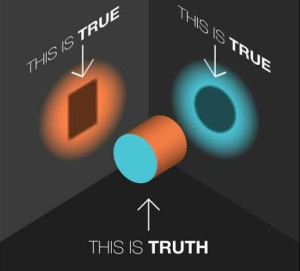
We could start to implement aspects of this care immediately. No Research required. I learned in Medical School the importance of listening to my Patients. Somehow, the Psychiatric World felt immune to this important rule in developing a Healthy Therapeutic Relationship. Yes, unshared reality exists with Patients and Psychiatrists. It does  not negate the essential therapeutic role of being heard. Not simply answering the Biomedical Model questions that railroad you into a corner. I learned about the importance of open questions in Medical School. As a patient in Psychiatry, I am shocked at the high percentage of closed, assuming, judgmental questions I have been asked to answer – especially when in crisis. POD offers the ability to compassionately review the unshared reality. I challenge the assumption that the Clinician’s view of Reality is the only viable one on offer in this world. Truth looks differently from each perspective.
not negate the essential therapeutic role of being heard. Not simply answering the Biomedical Model questions that railroad you into a corner. I learned about the importance of open questions in Medical School. As a patient in Psychiatry, I am shocked at the high percentage of closed, assuming, judgmental questions I have been asked to answer – especially when in crisis. POD offers the ability to compassionately review the unshared reality. I challenge the assumption that the Clinician’s view of Reality is the only viable one on offer in this world. Truth looks differently from each perspective.
Ricky Martin, Cup Of Life.
“Here we Go. Allez, Allez, Allez. Go, Go, Go! Allez, Allez, Allez.”
Cheers!
 Addendum September 21, 2015:
Addendum September 21, 2015:
Thinking about the above picture where Truth as a 3D tube gives off true shadows shaped as either a 2 Dimensional square or circle, depending on the perspective. Imagine Truth originating from the 4th Dimension, 5D or even higher? It is quite difficult for our minds to be able to conceptualize. Reality will be perceived within the parameters of our physical and mental abilities to perceive. It is not surprising the grand variety of perceptions that exist among us. Food for thought.
It is not about right or wrong, but many versions of right.